Recent scientific advancements have unveiled a previously unknown self-sustaining molecular circuit operating within pancreatic ductal adenocarcinoma (PDAC), the most prevalent and lethal form of pancreatic cancer, offering a novel perspective on its aggressive progression and potential avenues for therapeutic intervention. Pancreatic ductal adenocarcinoma stands as one of oncology’s most formidable challenges, distinguished by its high mortality rate, often attributed to late-stage diagnosis and inherent resistance to conventional treatments. Despite decades of intensive research, patient outcomes for PDAC remain stark, with a five-year survival rate that lags significantly behind most other major cancers. A predominant characteristic of PDAC is the frequent mutation of the KRAS gene, an oncogene that acts as a central switch in cellular growth and division pathways. While the development of targeted therapies specifically aimed at inhibiting mutant KRAS has marked a significant milestone, these interventions often encounter a critical hurdle: many PDAC tumors eventually develop mechanisms to bypass or evade these targeted agents, leading to relapse and continued disease progression. This inherent adaptability of pancreatic cancer cells underscores the urgent need for a deeper understanding of its underlying molecular architecture and the identification of alternative, synergistic therapeutic strategies that can overcome such resistance mechanisms. The pursuit of combination therapies, designed to simultaneously target multiple molecular vulnerabilities, represents a promising frontier in the effort to dismantle the complex machinery driving this aggressive malignancy.
In a pivotal development, research conducted in 2023 by scientists associated with Cold Spring Harbor Laboratory (CSHL) under the leadership of Professor Adrian Krainer illuminated the role of a protein designated SRSF1 as an early instigator of PDAC tumor genesis. This initial discovery provided a crucial molecular anchor point for subsequent investigations into the intricate signaling networks governing pancreatic cancer development. Building upon the foundational dataset generated by that prior study, a subsequent inquiry, spearheaded by former CSHL graduate student Alexander Kral, embarked on a more granular examination. This deeper dive revealed that SRSF1 does not operate in isolation but rather functions as an integral component within a sophisticated, tripartite molecular system. This newly identified circuit, far from being a mere collection of interacting molecules, appears to orchestrate the escalation of the cancer’s aggressive phenotype, actively driving its progression.
Dr. Kral elaborated on the hypothesis that guided their investigation, stating, "Our foundational theory posited that certain molecular alterations induced by elevated levels of SRSF1 were directly contributing to the accelerated tumor growth we had previously observed." This directed their focus towards pinpointing specific downstream effectors within the SRSF1 pathway. "We systematically narrowed our search to a particular molecule that we hypothesized could serve as a crucial driver within this pathway: Aurora kinase A, or AURKA," Kral explained. The ensuing research confirmed this suspicion, revealing AURKA’s central role. "What we uncovered was its participation in a complex regulatory circuit," he continued, "a system that encompasses not only AURKA and SRSF1 but also incorporates another well-established oncogene, MYC." This revelation transformed the understanding of SRSF1’s singular role into a more expansive view of a highly interconnected and mutually reinforcing oncogenic network.
Deconstructing the Self-Reinforcing Cancer Circuit
The intricate architecture of this newly identified molecular circuit relies on a series of interdependent regulatory steps, creating a self-sustaining loop that perpetually fuels cancer progression. At the nexus of this system, SRSF1 exerts its influence over AURKA primarily by modulating its genetic expression through a sophisticated biological mechanism known as alternative splicing. Alternative splicing is a fundamental post-transcriptional process in eukaryotic cells, allowing a single gene to encode multiple protein variants (isoforms) by selectively including or excluding specific segments of RNA (exons) during the messenger RNA (mRNA) maturation process. In this context, SRSF1’s manipulation of AURKA’s alternative splicing patterns leads to a significant upregulation in the production of specific AURKA isoforms, effectively increasing the overall cellular levels of the AURKA protein.
The elevated presence of AURKA, in turn, plays a crucial role in stabilizing and safeguarding the MYC protein from degradation. MYC is a potent transcription factor, an oncogene frequently amplified or dysregulated in a wide array of human cancers, known for its profound influence on cell proliferation, growth, and metabolism. Its stability is tightly regulated, and its increased persistence due to AURKA’s protective action amplifies its oncogenic potential. The heightened stability and activity of MYC then completes the regulatory loop by directly stimulating the transcriptional machinery responsible for the increased production of SRSF1. This cyclical activation – SRSF1 influencing AURKA, AURKA protecting MYC, and MYC boosting SRSF1 – establishes a robust, self-reinforcing feedback mechanism that continuously propels the cancer-promoting cellular environment, making it exceptionally aggressive and difficult to halt.
Professor Krainer highlighted the groundbreaking nature of this discovery: "While individual components or ‘bits and pieces’ of this circuit had been alluded to or partially characterized in prior research, the complete, integrated picture of their interdependency and self-reinforcing nature remained elusive until now." He emphasized the critical turning point in their understanding: "Once we definitively established the involvement of alternative splicing of AURKA as a central regulatory node within this circuit, it opened up entirely new avenues for exploring targeted interventions designed to disrupt its function." This comprehensive understanding of the circuit’s mechanics is paramount for designing effective therapeutic strategies that can precisely dismantle its oncogenic drive.
The Strategic Disruption: Collapsing the Circuit with a Single Target
Armed with this newfound understanding of the self-reinforcing circuit, the research team embarked on developing a targeted intervention strategy. Their approach centered on creating an antisense oligonucleotide (ASO) specifically engineered to modulate the alternative splicing of AURKA. Antisense oligonucleotides are short, synthetic strands of nucleic acids designed to bind to specific RNA sequences, thereby altering gene expression. This therapeutic modality leverages the cell’s natural RNA processing machinery to achieve highly precise gene modulation. The Krainer lab possesses extensive expertise in the development and application of ASOs, a testament to their pioneering work in the field. Notably, this group was instrumental in the creation of Spinraza (nusinersen), the first-ever FDA-approved treatment for spinal muscular atrophy (SMA), a devastating neurodegenerative disease. The success of Spinraza underscores the immense potential of ASO technology in addressing previously untreatable conditions by directly intervening at the RNA level to correct molecular defects.
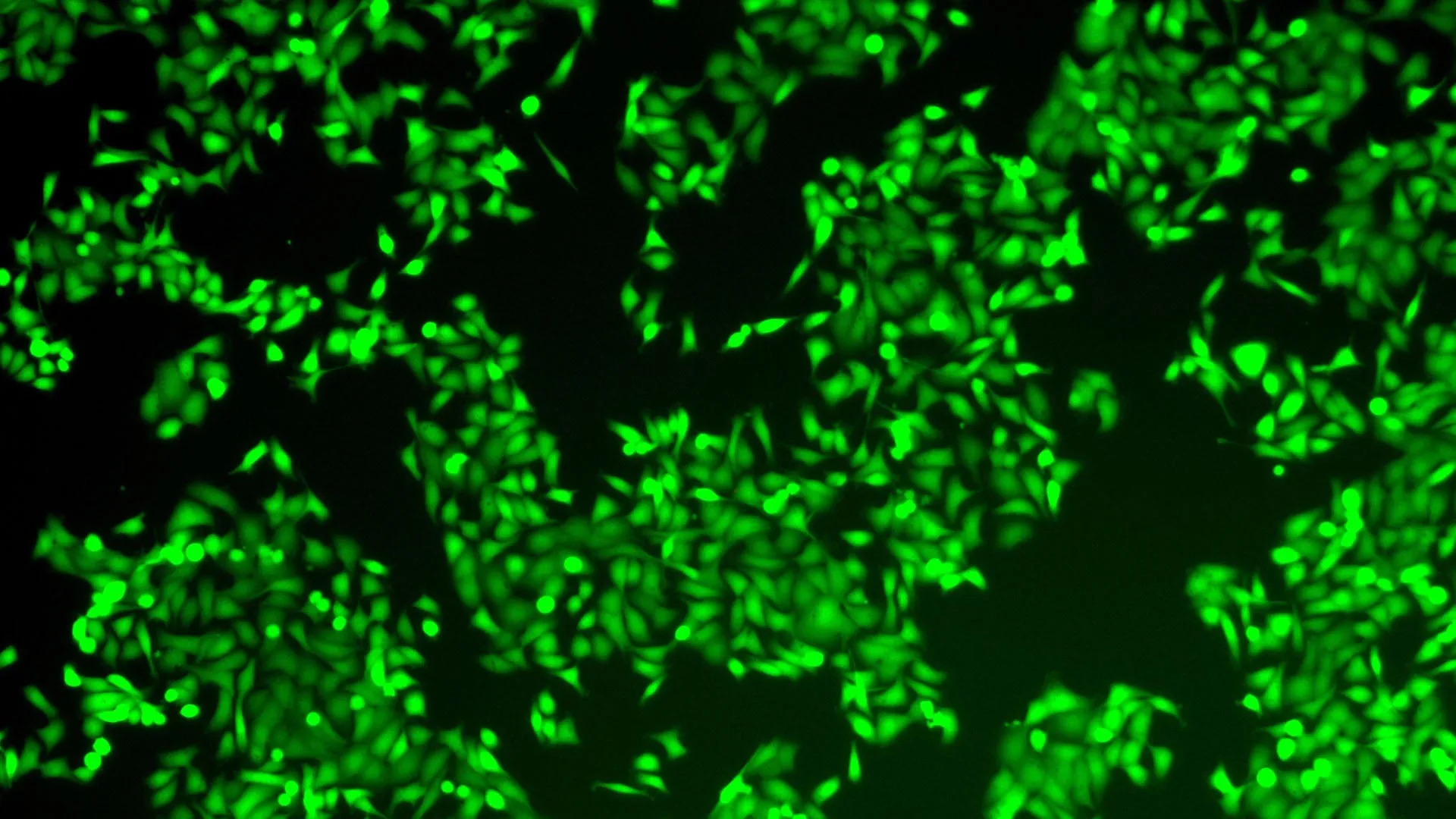
Based on their prior findings and the established mechanism of ASO action, the researchers initially anticipated that the newly designed ASO would specifically block the aberrant splicing of AURKA, thereby reducing the production of its oncogenic isoforms. However, in experiments conducted using pancreatic cancer cells, the observed effects were far more profound and dramatic than initially predicted. Instead of merely inhibiting AURKA splicing, the ASO treatment instigated a complete collapse of the entire cancer-driving circuit. The downstream consequences were immediate and catastrophic for the malignant cells: tumor cells experienced a significant loss of viability, a precursor to cell death, and critically, activated apoptosis – a highly regulated form of programmed cell death. This outcome suggests that the circuit, once disrupted at a single, critical node, becomes unstable and unable to sustain itself, leading to the rapid demise of the cancerous cells.
Professor Krainer succinctly captured the efficiency and impact of this targeted intervention: "It’s akin to achieving multiple objectives with a single, precise action – effectively ‘killing three birds with one stone.’" He elaborated on the significance: "SRSF1, AURKA, and MYC are all well-established oncogenes, each individually recognized for their contributions to the progression and aggressiveness of PDAC. The remarkable aspect of our discovery is that by solely targeting the alternative splicing of AURKA with our specialized ASO, we concurrently observe the dramatic reduction or loss of the other two critical oncogenic molecules within the circuit." This simultaneous incapacitation of multiple key oncogenes through a single point of intervention represents a highly advantageous therapeutic strategy. It not only offers the potential for greater efficacy by disrupting redundant pathways but also reduces the likelihood of resistance mechanisms emerging that might circumvent single-target therapies.
Implications and Future Directions for Pancreatic Cancer Therapies
The identification and successful disruption of this self-reinforcing molecular loop in PDAC represent a significant conceptual leap in cancer research. It shifts the paradigm from solely targeting individual oncogenes to understanding and dismantling interconnected oncogenic networks. The implications of this discovery are profound, potentially paving the way for fundamentally new therapeutic strategies for pancreatic cancer, a disease notoriously resistant to current approaches. By collapsing an entire oncogenic circuit, rather than merely inhibiting a single component, this approach may offer a more robust and durable therapeutic response, effectively overcoming the adaptive resistance that frequently plagues targeted cancer therapies.
The Krainer lab remains actively engaged in the ongoing refinement and optimization of this promising ASO. While the potential for its direct clinical application in human patients remains a distant prospect, requiring extensive preclinical validation, rigorous toxicology studies, and multiple phases of clinical trials, the foundational nature of this research cannot be overstated. Professor Krainer emphasized this critical progression, drawing parallels to the developmental trajectory of Spinraza. That groundbreaking drug, now saving thousands of lives globally, similarly originated from intensive foundational research and iterative refinement in the laboratory. The current work on the AURKA-targeting ASO is following an analogous path, representing a crucial early stage in the arduous journey from basic scientific discovery to a transformative medical intervention.
The future outlook for this research is multi-faceted. Further investigations will focus on enhancing the potency, specificity, and delivery mechanisms of the ASO. ASOs, while powerful, face challenges in systemic delivery to solid tumors and ensuring their stability and cellular uptake without off-target effects. Research into novel encapsulation methods, such as lipid nanoparticles, or localized delivery techniques could be crucial for their successful translation to pancreatic cancer treatment. Moreover, exploring potential combination therapies is a critical next step. This ASO could be investigated in conjunction with existing KRAS inhibitors, chemotherapy agents, or immunotherapies. Such synergistic combinations might not only enhance efficacy but also broaden the patient population that could benefit, offering a comprehensive assault on the multifaceted nature of PDAC.
Beyond pancreatic cancer, the principles elucidated by this discovery could have broader ramifications. The existence of self-reinforcing oncogenic loops may be a common feature across various cancer types. Understanding and identifying such circuits in other malignancies could unlock similar "Achilles’ heels," offering a universal strategy for collapsing cancer’s inherent growth engines. This work contributes to the growing field of systems biology in oncology, moving towards a more holistic understanding of cancer as a complex, adaptive system rather than a collection of isolated defects. Ultimately, with continued dedication and further refinement, this pioneering research holds the distinct promise of contributing to the development of a novel, highly effective, and potentially life-saving treatment strategy for pancreatic cancer, offering a beacon of hope where therapeutic options are desperately needed.








