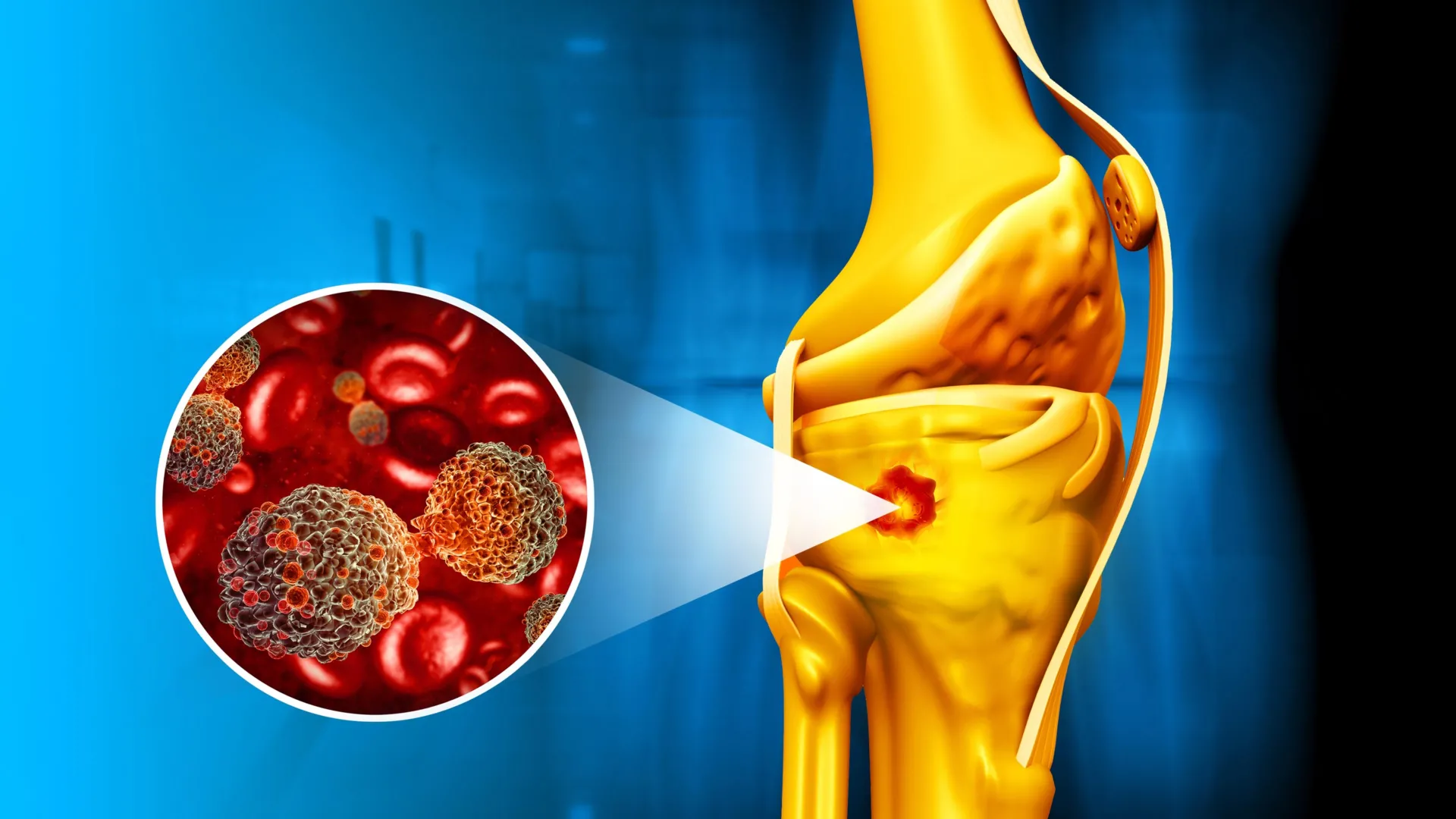
A groundbreaking development in nanomedicine offers a dual-pronged attack against bone cancer, simultaneously eradicating malignant cells and fostering the regeneration of healthy tissue. This innovative approach centers on a novel magnetic nanocomposite engineered to precisely target cancerous lesions through localized heat generation while concurrently promoting bone repair, presenting a significant advance in the treatment paradigm for osteosarcoma and other bone malignancies.
Bone cancer, encompassing primary tumors like osteosarcoma and metastatic lesions originating from other parts of the body, represents a formidable challenge in oncology. Current therapeutic strategies often involve a combination of surgery, chemotherapy, and radiation, which, while effective to varying degrees, frequently carry substantial side effects, including systemic toxicity, compromised bone integrity, and a risk of recurrence. Surgical resection, particularly for large or complex tumors, can lead to significant functional impairment and necessitate extensive reconstructive procedures. The inherent difficulties in achieving complete tumor eradication while preserving healthy bone tissue underscore an urgent demand for more localized, less invasive, and functionally restorative treatment modalities.
The research, conducted by an international team and detailed in a recent publication, introduces a sophisticated core-shell material designed to address these critical unmet needs. At its heart lies a core of iron oxide nanoparticles, renowned for their superparamagnetic properties. This core is meticulously encapsulated within a thin, protective layer of bioactive glass, a class of materials celebrated for their capacity to integrate with and stimulate the regeneration of bone tissue. This ingenious architectural design enables the nanocomposite to harness the power of magnetic fields for targeted hyperthermia—a process where elevated temperatures are used to destroy cancer cells—while simultaneously providing a scaffold and chemical cues for osteogenesis, the formation of new bone.
Historically, the scientific community has grappled with the inherent incompatibility of integrating robust magnetic responsiveness with strong biological activity within a single material. Achieving both high magnetization, crucial for effective hyperthermia, and potent bioactivity, essential for bone regeneration, has presented a persistent hurdle. Diverse material properties, processing requirements, and often conflicting chemical compositions have typically forced a compromise between these two vital functions. The breakthrough achieved by this research lies in successfully overcoming this long-standing challenge, demonstrating that it is indeed possible to engineer a single material capable of delivering both powerful magnetic heating and significant bone-healing properties.
Dr. Ângela Andrade, a lead author involved in the study, highlighted the transformative potential of these advancements. "Magnetic bioactive nanocomposites hold immense promise for bone cancer therapy," Dr. Andrade stated, "because they possess the unique capability to simultaneously ablate tumors through precisely controlled magnetic hyperthermia and actively support the growth of new, healthy bone. Our findings conclusively demonstrate the feasibility of achieving both high magnetization and strong bioactivity within the same nanocomposite, a significant scientific and engineering accomplishment that addresses a critical need in the field." This confluence of capabilities points towards a future where treatment is not just about eradicating disease but also about restoring function and quality of life.
To rigorously assess the material’s potential performance within a biological environment, the researchers subjected the nanocomposites to simulated physiological conditions. By immersing the particles in simulated body fluid (SBF), a solution designed to mimic the inorganic ion composition of human blood plasma, the team observed the material’s interaction with the biological milieu. Crucially, under these conditions, the nanocomposites rapidly facilitated the formation of apatite, a crystalline calcium phosphate mineral that constitutes the primary inorganic component of natural bone. This swift and robust mineralization process is a strong indicator of the material’s excellent osteoconductive properties, suggesting that upon implantation, it would readily integrate with existing bone tissue, forming a stable and regenerative interface.
Further refinement of the nanocomposite formulations revealed significant variations in performance. Among the different compositions evaluated, a particular version enriched with a higher concentration of calcium ions distinguished itself. This calcium-enhanced formulation exhibited not only the fastest rate of apatite formation but also demonstrated the most potent magnetic response. "The formulation incorporating an elevated calcium content consistently outperformed others," Dr. Andrade elaborated, "displaying both accelerated mineralization kinetics and a superior magnetic heating capacity. This makes it an exceptionally promising candidate for a broad spectrum of biomedical applications, particularly those requiring efficient bone regeneration and targeted hyperthermia." The strategic manipulation of elemental composition, therefore, proved pivotal in optimizing the material’s multifunctional attributes.
The core function of the iron oxide nanoparticles in this composite is to serve as highly efficient generators of heat when subjected to an alternating magnetic field (AMF). This phenomenon, known as magnetic hyperthermia, allows for the precise, localized delivery of thermal energy directly to the tumor site. When the AMF is applied, the magnetic nanoparticles within the tumor tissue absorb energy, converting it into heat. This localized temperature elevation, typically between 42°C and 47°C, is sufficient to induce apoptosis (programmed cell death) or necrosis in cancer cells, which are generally more sensitive to heat than healthy cells. The beauty of this approach lies in its non-invasive nature and the ability to selectively target malignant tissue, thereby minimizing collateral damage to surrounding healthy bone and soft tissues—a stark contrast to the widespread effects of conventional chemotherapy or radiation.
Concurrently, the bioactive glass shell plays an equally critical role in the healing and regenerative aspect of the therapy. Bioactive glasses are known for their ability to bond directly with bone and stimulate osteoblast activity, the cells responsible for new bone formation. Upon contact with physiological fluids, the bioactive glass surface undergoes a series of reactions, leading to the formation of a silica-rich gel layer and subsequently the precipitation of a carbonated apatite layer. This apatite layer provides a biocompatible interface that encourages the adhesion, proliferation, and differentiation of osteoprogenitor cells, effectively guiding and accelerating the natural bone regeneration process. Thus, the nanocomposite is not merely destroying cancer; it is actively participating in the reconstruction of the damaged skeletal architecture, offering a holistic solution to a complex medical problem.
"This investigation has provided profound new insights into the intricate relationship between the surface chemistry and overall structure of magnetic biomaterials and their resultant performance," Dr. Andrade noted. "These findings are crucial, as they pave the way for the development of increasingly sophisticated and multifunctional materials that are both inherently safe and clinically efficacious. The ability to fine-tune these properties at the nanoscale opens up unprecedented opportunities for future therapeutic interventions." The detailed understanding of these fundamental interactions is paramount for translating laboratory discoveries into viable clinical tools.
The broader implications of this research extend far beyond the immediate context of bone cancer treatment. It represents a significant stride forward in the burgeoning fields of smart nanomaterials, oncology, and regenerative medicine. By seamlessly integrating robust magnetic performance with bone-friendly bioactivity, these advanced nanocomposites offer a compelling vision for future therapies. Such therapies could potentially involve a single, minimally invasive procedure capable of not only eradicating bone tumors but also simultaneously restoring damaged skeletal tissue. This integrated approach promises to reduce patient burden, accelerate recovery times, and improve long-term functional outcomes.
Looking ahead, the successful translation of these magnetic nanocomposites into clinical practice will necessitate further rigorous evaluation. In vivo studies in animal models will be critical to assess long-term biocompatibility, systemic effects, degradation profiles, and the precise efficacy of combined hyperthermia and regeneration in a living system. Challenges such as controlling the precise dosage, optimizing magnetic field parameters for human application, and ensuring scalability of production for clinical use will need to be addressed. Furthermore, regulatory hurdles, including safety assessments and approval processes, will be substantial.
Despite these challenges, the potential for these multifunctional nanoparticles is immense. They could offer a paradigm shift for patients suffering from osteosarcoma, metastatic bone disease, and even complex bone fractures or defects requiring enhanced regeneration. The ability to deliver targeted therapy with simultaneous regenerative capabilities opens doors to personalized medicine approaches, where treatment can be tailored to the specific characteristics of an individual’s tumor and bone defect. Moreover, this platform could potentially be expanded to incorporate drug delivery capabilities, allowing for the co-delivery of chemotherapeutic agents directly to the tumor, further enhancing treatment efficacy while reducing systemic toxicity. The convergence of nanotechnology, materials science, and biomedical engineering demonstrated in this research heralds a new era for therapeutic interventions, promising more effective, less invasive, and restorative treatments for some of the most challenging medical conditions.







