Groundbreaking neuroscientific investigations reveal a compelling association between the debilitating neurological disorder of temporal lobe epilepsy and the premature aging of specific brain cells, suggesting a potential paradigm shift in treatment strategies. Researchers at Georgetown University Medical Center have demonstrated that the selective elimination of these senescent, or "zombie," cells in preclinical models not only significantly diminished seizure frequency but also markedly improved memory function and, remarkably, prevented the onset of epilepsy in a subset of subjects. This innovative approach, termed senotherapy, employed both sophisticated genetic manipulation and a targeted pharmacological intervention, opening a new frontier for addressing a condition that profoundly impacts millions globally.
Epilepsy, a chronic neurological disorder characterized by recurrent, unprovoked seizures, affects an estimated 50 million individuals worldwide. The condition manifests in diverse forms, each presenting unique challenges, but a common thread is the significant impact on quality of life, cognitive function, and mental well-being. Temporal Lobe Epilepsy (TLE) stands as one of the most prevalent and therapeutically challenging variants, often characterized by complex partial seizures originating in the temporal lobes of the brain. Beyond the overt seizure events, TLE frequently leads to a spectrum of cognitive deficits, including memory impairment, executive dysfunction, and mood disorders, further burdening patients and their caregivers. A critical unmet need in epilepsy care is the substantial proportion of individuals — approximately one-third — whose seizures remain refractory to conventional anti-epileptic medications, leaving surgical intervention as often the only recourse. This new research offers a compelling alternative or adjunctive strategy, moving beyond mere symptom management toward addressing fundamental pathophysiological mechanisms.
The concept of cellular senescence, a state in which cells cease dividing but remain metabolically active, secreting a complex array of pro-inflammatory and tissue-damaging molecules, has garnered increasing attention across various fields of medicine. Often colloquially referred to as "zombie cells," senescent cells accumulate with age and in response to various stressors, contributing to chronic inflammation, tissue dysfunction, and the progression of numerous age-related diseases, from cardiovascular conditions to neurodegenerative disorders. The emerging field of senotherapeutics, encompassing senolytics (drugs that selectively kill senescent cells) and senomorphics (drugs that modulate their harmful secretions), represents a burgeoning area of therapeutic development. The application of this concept to a neurological disorder like epilepsy, traditionally viewed through the lens of aberrant neuronal excitability, marks a significant conceptual leap.
Dr. Patrick A. Forcelli, a distinguished professor and chair of Georgetown School of Medicine’s Department of Pharmacology & Physiology, and the Jerome H. Fleisch & Marlene L. Cohen Endowed Professor of Pharmacology, articulated the profound clinical implications of these findings. "A substantial portion of individuals living with epilepsy do not achieve seizure freedom with current pharmacotherapies," Dr. Forcelli explained. "Our aspiration is that senotherapy, through the targeted removal of these senescent cells, could potentially reduce the necessity for invasive surgical procedures and/or enhance patient outcomes following such interventions." This statement underscores the potential for a paradigm shift in epilepsy management, offering hope to those for whom existing treatments have proven inadequate.
Temporal lobe epilepsy can originate from a heterogeneous array of underlying etiologies. These include traumatic brain injuries, cerebrovascular accidents such as stroke, infectious diseases like meningitis, the presence of brain tumors, congenital malformations of blood vessels, and specific inherited genetic predispositions. Despite this varied origin, TLE frequently converges on a common pathophysiological pathway that leads to its characteristic drug-resistant nature. Affecting approximately 40% of all epilepsy patients, TLE is the most common form of epilepsy that exhibits limited responsiveness to pharmacological agents, highlighting the urgent need for novel therapeutic avenues.
To elucidate the biological underpinnings of TLE, the research team embarked on an examination of donated human brain tissue. This tissue had been meticulously obtained from the temporal lobes of epilepsy patients undergoing surgical resection as part of their treatment. A comparative analysis against post-mortem samples acquired from individuals without a history of epilepsy revealed a striking disparity: the brain tissue from TLE patients exhibited a five-fold elevation in the presence of senescent glial cells. Glial cells, often overshadowed by neurons, are indispensable support cells within the central nervous system. They do not generate electrical signals themselves but perform critical functions including providing metabolic support, maintaining the blood-brain barrier, regulating neurotransmitter levels, and mediating immune responses. The discovery of an overwhelming accumulation of senescent glial cells in human TLE tissue provided a crucial biological anchor for the subsequent preclinical investigations. This finding suggested that glial cell dysfunction, driven by senescence, might not merely be a consequence of chronic seizures but a contributing factor to the epileptogenic process itself.
Building upon these pivotal observations in human tissue, the research team proceeded to investigate whether a similar accumulation of aging cells occurred in a meticulously developed mouse model designed to recapitulate key features of TLE. Within a mere two weeks following the brain injury that served as the initiating event for epilepsy in these animals, the researchers detected unequivocal increases in established markers of cellular aging, observable at both the gene expression and protein levels. This rapid onset of senescence following injury suggests that the pathological process might be an early event, potentially offering a critical window for therapeutic intervention.
The subsequent therapeutic interventions, aimed at eliminating these identified senescent cells, yielded substantial and encouraging results. The number of senescent cells within the brain tissue of treated mice was reduced by approximately 50%. This partial reduction proved remarkably effective. Treated mice demonstrated normalized performance on complex maze-based memory tasks, indicating a significant restoration of cognitive function. Furthermore, these animals experienced a demonstrably lower frequency of seizures. Most notably, about one-third of the treated mice were completely protected from the development of epilepsy, a profound outcome that points towards disease modification rather than mere symptom suppression. This protective effect suggests that early intervention to clear senescent cells might interrupt the epileptogenic cascade, preventing the establishment of chronic seizure activity.
The pharmacological intervention employed in the mouse model involved a strategic combination of two agents: dasatinib and quercetin. Dasatinib is a well-established targeted therapy, currently approved by the U.S. Food and Drug Administration (FDA) for the treatment of specific forms of leukemia. Its mechanism of action involves inhibiting various tyrosine kinases, crucial enzymes involved in cell growth and survival. Quercetin, a naturally occurring plant flavonoid abundant in fruits, vegetables, tea, and wine, possesses potent antioxidant and anti-inflammatory properties. This specific drug combination has been extensively utilized in preclinical animal studies to selectively eliminate senescent cells across a diverse range of disease models, showcasing its broad applicability as a senolytic agent.
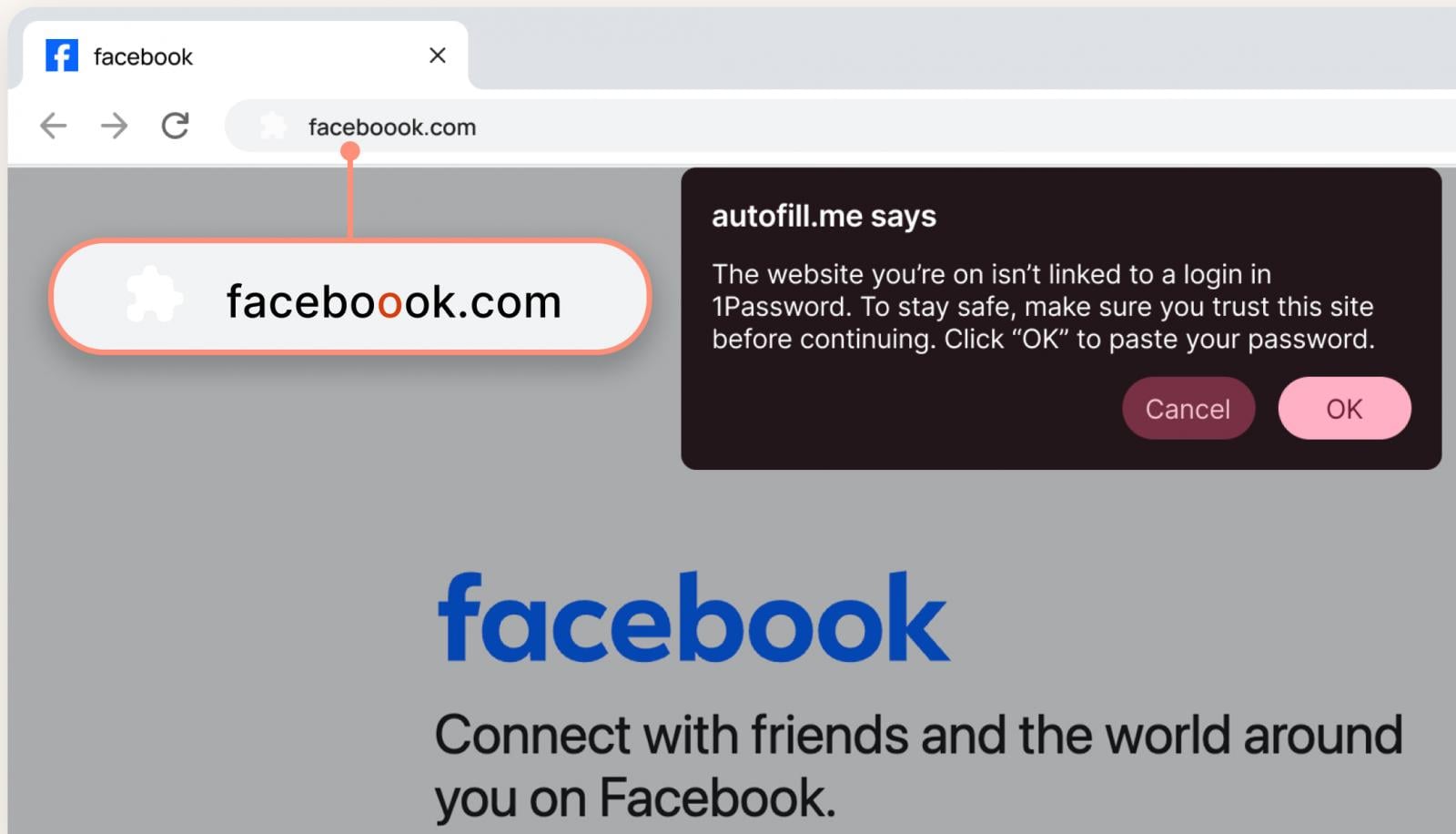
The researchers’ rationale for selecting these particular drugs was multifaceted and strategic. Both dasatinib and quercetin are already undergoing evaluation in early-phase clinical trials for other medical conditions, a factor that significantly de-risks their potential translation to epilepsy. Dr. Forcelli further emphasized that dasatinib’s existing FDA approval for leukemia means its safety profile in humans is extensively documented and well-understood. This pre-existing knowledge base could substantially accelerate the timeline for transitioning these findings from preclinical studies into clinical testing in individuals afflicted with epilepsy, circumventing lengthy early-phase safety evaluations.
The implications of this research extend far beyond the immediate context of epilepsy. Dr. Tahiyana Khan and David J. McFall, both first co-authors of the study and trainees in Dr. Forcelli’s laboratory, underscored that the aging of glial cells has recently been implicated not only in the physiological processes of normal brain aging but also in the pathogenesis of debilitating neurodegenerative conditions, prominently including Alzheimer’s disease. This intricate connection establishes a crucial bridge between epilepsy research and the broader efforts to combat age-related neurological decline, suggesting that targeting glial senescence might offer a common therapeutic strategy for a spectrum of brain disorders. This line of inquiry remains a central focus of their ongoing research endeavors.
Looking ahead, Dr. Forcelli articulated the strategic direction of their future investigations. "We are currently conducting studies utilizing other repurposed pharmaceutical agents that possess the capacity to influence cellular senescence, alongside explorations in additional rodent models of epilepsy," he stated. "Our overarching objective is to precisely delineate the critical temporal windows for intervention in epilepsy, with the ultimate ambition that these cumulative studies will culminate in the development of clinically viable treatments." Identifying these "critical windows" is paramount, as it could dictate the optimal timing for administering senotherapeutic agents to achieve maximal benefit, potentially preventing epileptogenesis if administered early after an inciting injury or mitigating disease progression in established cases.
The comprehensive study, published on December 22 in the esteemed journal Annals of Neurology, represents a collaborative effort from a multidisciplinary team at Georgetown University. In addition to Dr. Forcelli, Dr. Khan, and Mr. McFall, key authors included Abbas I. Hussain, Logan A. Frayser, Timothy P. Casilli, Meaghan C. Steck, Dr. Irene Sanchez-Brualla, Noah M. Kuehn, Michelle Cho, Dr. Jacqueline A. Barnes, Dr. Brent T. Harris, and Dr. Stefano Vicini. The authors collectively affirmed that they possess no personal financial interests directly related to the study, ensuring the integrity and objectivity of their groundbreaking work. This pivotal research received substantial financial backing from various grants provided by the National Institutes of Health (NIH), specifically R21NS125552, F99NS129108, T32NS041218, T32GM142520, F30NS143374-01, T32GM144880, and T3GM142520. Dr. Forcelli also benefits from additional support as the esteemed Jerome H. Fleisch & Marlene L. Cohen Endowed Professor of Pharmacology, further enabling his impactful contributions to neuropharmacology.
This research marks a significant departure from traditional approaches to epilepsy, which have largely focused on modulating neuronal excitability. By identifying cellular senescence, particularly in glial cells, as a key driver of epileptogenesis and cognitive dysfunction, the Georgetown team has unveiled a novel, targetable pathway. The potential to repurpose existing, well-characterized drugs like dasatinib, combined with the natural compound quercetin, offers a faster track to clinical trials and, ultimately, to new hope for millions suffering from drug-resistant epilepsy and its devastating cognitive consequences. The convergence of epilepsy with broader neurodegenerative processes through the lens of cellular aging also suggests a unifying therapeutic strategy that could transform the treatment landscape for a range of intractable brain disorders.