A significant reevaluation of the therapeutic mechanisms underlying commonly prescribed stimulant medications for Attention-Deficit/Hyperactivity Disorder (ADHD) is underway following groundbreaking research. Contrary to long-held assumptions that these drugs directly enhance brain networks governing attention, recent scientific inquiry suggests their primary influence lies in modulating systems related to reward and wakefulness, fundamentally altering our understanding of their efficacy and potential implications for patient care. This revelation prompts a critical reexamination of diagnostic approaches, treatment strategies, and the broader societal implications of stimulant use, particularly concerning sleep health.
For decades, prescription stimulant medications, including compounds like methylphenidate (Ritalin) and amphetamines (Adderall), have been the cornerstone of pharmacological treatment for ADHD. Their widespread use is undeniable; in the United States alone, an estimated 3.5 million children between the ages of 3 and 17 receive medication for the neurodevelopmental disorder. This figure has steadily climbed in tandem with increasing diagnostic rates, solidifying stimulants’ perceived role as direct enhancers of cognitive functions, specifically attention. The prevailing scientific consensus posited that these agents primarily modulated neurotransmitter systems, such as dopamine and norepinephrine, to directly strengthen brain regions responsible for sustained focus and executive function. However, a recent comprehensive study from Washington University School of Medicine in St. Louis now challenges this foundational understanding, proposing an alternative, more nuanced model of their therapeutic action.
The research, spearheaded by Dr. Benjamin Kay and Dr. Nico U. Dosenbach, represents a pivotal moment in ADHD pharmacology. Published in Cell, their findings suggest that the benefits observed with stimulant use—improved performance and reduced hyperactivity—are not a direct consequence of sharpened attention networks. Instead, these medications appear to exert their primary effects on neural pathways associated with arousal, wakefulness, and the brain’s intricate reward system. This means that rather than directly "fixing" attention deficits, stimulants might make individuals feel more alert and find tasks more intrinsically rewarding, thereby indirectly facilitating engagement and focus. The study also remarkably identified brain activity patterns in stimulant users that mirrored the restorative effects of adequate sleep, counteracting the typical neural signatures of sleep deprivation.
Dr. Kay, a child neurologist who frequently prescribes these medications, articulated the dissonance between established teaching and the new data. He noted, "I’ve always been taught that they facilitate attention systems to give people more voluntary control over what they pay attention to. But we’ve shown that’s not the case. Rather, the improvement we observe in attention is a secondary effect of a child being more alert and finding a task more rewarding, which naturally helps them pay more attention to it." This reinterpretation has profound implications, underscoring the necessity of integrating sleep quality into the holistic evaluation and management of children diagnosed with ADHD.
To meticulously investigate the neural underpinnings of stimulant action, the research team utilized resting-state functional magnetic resonance imaging (fMRI) data from a substantial cohort of 5,795 children aged 8 to 11, drawn from the Adolescent Brain Cognitive Development (ABCD) Study. The ABCD study is an extensive, multi-site longitudinal project meticulously tracking the brain development of over 11,000 children across the United States. Resting-state fMRI captures spontaneous brain activity when individuals are not engaged in a specific task, providing insights into baseline neural connectivity. By comparing brain connectivity patterns in children who had taken prescription stimulants on the day of their scan with those who had not, the researchers uncovered compelling distinctions. Children administered stimulants exhibited markedly stronger activity in brain regions critically involved in arousal and wakefulness, alongside areas implicated in predicting the potential reward of an activity. Crucially, in contrast to prevailing theories, the scans did not reveal any significant increases in activity within the neural networks traditionally associated with direct attentional control.
To validate these initial findings and eliminate confounding variables inherent in observational studies, the researchers conducted a smaller, controlled experiment involving five healthy adults who did not have ADHD and were not regular stimulant users. Each participant underwent resting-state fMRI scans both before and after receiving a single dose of a stimulant. This within-subject design allowed for precise tracking of medication-induced changes in brain connectivity. The results from this adult cohort unequivocally corroborated the initial findings from the children’s study: the medications primarily activated networks associated with reward and arousal, rather than directly stimulating attention networks.
Dr. Dosenbach elucidated the practical implications of these findings, stating, "Essentially, we found that stimulants pre-reward our brains and allow us to keep working at things that wouldn’t normally hold our interest—like our least favorite class in school, for example." This "pre-rewarding" mechanism suggests that stimulants render typically arduous or uninteresting tasks more engaging and palatable, thereby increasing persistence and focus. This model offers a compelling explanation for how stimulants ameliorate hyperactivity, a phenomenon that has long posed a paradoxical challenge to the direct attention hypothesis. Hyperactivity, often characterized by fidgeting and an inability to remain seated, can be reinterpreted as a behavioral manifestation of disinterest or a lack of reward from the immediate task. By increasing the perceived reward of these activities, stimulants might enable children to maintain engagement and stillness more effectively, as they are less compelled to seek more stimulating alternatives.
Further analysis within the ABCD study cohort revealed practical benefits associated with stimulant use. Children with ADHD who were taking stimulant medications generally reported higher school grades, according to parent assessments, and demonstrated superior performance on cognitive tests compared to their counterparts with ADHD who were not receiving medication. These improvements were most pronounced in children exhibiting more severe ADHD symptoms, indicating a dose-response or severity-response relationship.
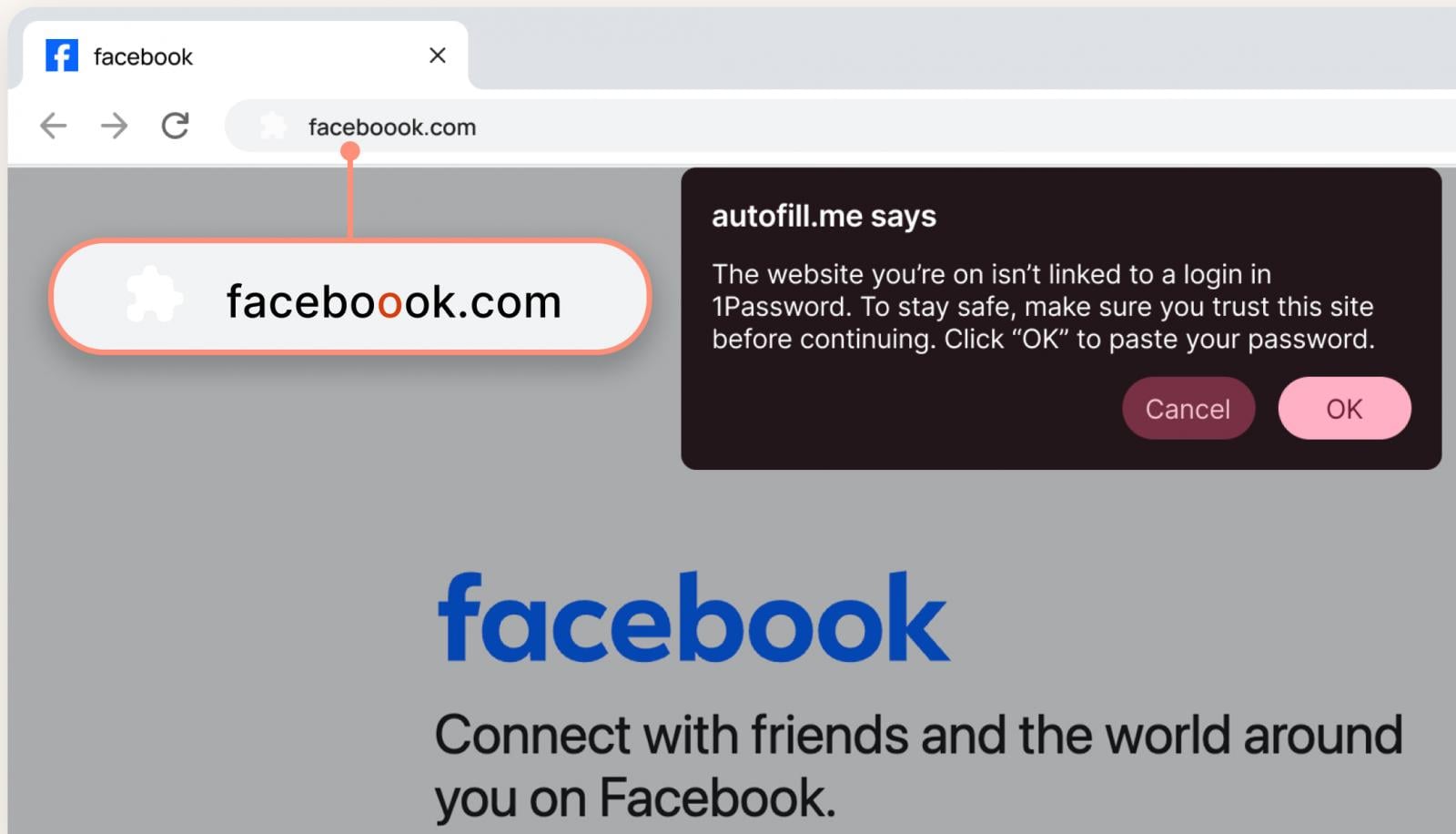
However, the benefits were not universally observed. A particularly illuminating finding emerged concerning sleep patterns. Among participants who consistently slept less than the recommended nine or more hours per night, those who took stimulants achieved better academic outcomes than their sleep-deprived peers who were not medicated. Conversely, in neurotypical children who were already obtaining sufficient sleep, stimulant use was not associated with improved cognitive performance. This observation highlights a critical interplay: the link between stimulants and enhanced cognitive function appeared predominantly in children diagnosed with ADHD or in those experiencing chronic sleep insufficiency, irrespective of an ADHD diagnosis. Dr. Dosenbach summarized this interaction concisely: "We saw that if a participant didn’t sleep enough, but they took a stimulant, the brain signature of insufficient sleep was erased, as were the associated behavioral and cognitive decrements."
While these findings illuminate the mechanisms of efficacy, they also introduce a significant cautionary note regarding potential long-term consequences. The ability of stimulants to mask the cognitive and behavioral deficits arising from sleep deprivation raises serious concerns. Dr. Kay emphasized, "Not getting enough sleep is always bad for you, and it’s especially bad for kids." Chronic sleep deprivation in children can manifest symptoms that closely mimic ADHD, including difficulties with attention, concentration, and declining academic performance. In some instances, this phenotypic overlap could lead to a misdiagnosis of ADHD when the root cause is fundamentally a sleep disorder. Stimulant medications, by artificially enhancing alertness and task engagement, might create a deceptive illusion of improvement, effectively obscuring the underlying sleep deficit and exposing children to the pervasive, long-term health risks associated with chronic sleep loss. This underscores the urgent need for clinicians to meticulously assess sleep hygiene and address any sleep disturbances during the comprehensive evaluation process for ADHD.
The findings from this groundbreaking research compel a re-evaluation of current diagnostic paradigms and therapeutic approaches for ADHD. If stimulants do not directly target attention networks, future research must delve deeper into the precise neural alterations characteristic of ADHD. This research also opens new avenues for exploring non-pharmacological interventions that might target reward and wakefulness systems, potentially offering alternative or supplementary treatment modalities.
Drs. Dosenbach and Kay advocate for continued research into the long-term neurological impacts of stimulant administration. They postulate that stimulants might possess a restorative capacity, potentially activating the brain’s waste-clearing systems during wakefulness. Conversely, the chronic use of these medications to compensate for persistent sleep deficits could engender unforeseen and potentially lasting neurological harm. The intricate relationship between medication, sleep, and cognitive function demands further longitudinal studies to fully comprehend the implications of these new insights for brain health and development. This evolving understanding of stimulant mechanisms necessitates a more holistic, personalized, and informed approach to ADHD diagnosis and treatment, prioritizing comprehensive patient well-being beyond symptomatic relief.