Ibuprofen, a pharmaceutical staple found in medicine cabinets worldwide, is predominantly recognized for its efficacy in alleviating pain and reducing inflammation. However, a growing body of scientific inquiry suggests that its pharmacological influence may extend beyond symptomatic relief, prompting researchers to explore its potential as a modulator of cancer risk across various malignancies. This evolving perspective could reshape preventative strategies, although experts emphasize the necessity of rigorous validation and careful consideration of associated risks.
The global burden of cancer continues to rise, necessitating a multifaceted approach to prevention, early detection, and treatment. While significant advancements have been made in therapeutic interventions, the search for accessible and effective chemopreventive agents remains a critical area of research. In this context, existing medications with well-understood pharmacological profiles, often termed "repurposed drugs," are gaining increasing attention. Ibuprofen, with its widespread use and established anti-inflammatory properties, presents an intriguing candidate for such investigation. The connection between chronic inflammation and the initiation and progression of cancer is a well-established paradigm in oncology, providing a foundational rationale for examining the role of anti-inflammatory compounds.
The Anti-Inflammatory Paradigm in Carcinogenesis
Chronic inflammation is a recognized hallmark of cancer, contributing to tumor initiation, promotion, progression, and metastasis. Prolonged inflammatory responses create a microenvironment conducive to oncogenesis through several mechanisms. Inflammatory cells release reactive oxygen and nitrogen species, leading to DNA damage and genetic mutations. They also secrete a plethora of cytokines, chemokines, and growth factors that stimulate cell proliferation, inhibit apoptosis (programmed cell death), promote angiogenesis (new blood vessel formation to feed tumors), and facilitate immune evasion. This intricate interplay between inflammatory mediators and cellular processes underscores why modulating inflammatory pathways could offer a viable strategy for cancer prevention.
Ibuprofen belongs to the class of non-steroidal anti-inflammatory drugs (NSAIDs), a group of compounds primarily known for their ability to suppress inflammation. The historical link between NSAIDs and cancer prevention is not a novel concept. Decades ago, clinical observations highlighted a reduced incidence of certain cancers, particularly colorectal malignancies, among individuals regularly using specific NSAIDs. This early evidence spurred extensive research into the chemopreventive potential of these widely prescribed and over-the-counter medications.
Pharmacological Mechanism: Targeting Cyclooxygenases
The primary mechanism by which NSAIDs, including ibuprofen, exert their anti-inflammatory and analgesic effects involves the inhibition of cyclooxygenase (COX) enzymes. There are two main isoforms: COX-1 and COX-2.
COX-1 is constitutively expressed in most tissues and plays vital "housekeeping" roles. It is responsible for producing prostaglandins that protect the gastric mucosa, regulate renal blood flow, and facilitate platelet aggregation for blood clotting. Inhibition of COX-1, while effective in reducing inflammation, can lead to adverse effects such as gastrointestinal irritation, ulcers, and bleeding.
COX-2, on the other hand, is largely inducible, meaning its expression is significantly upregulated during inflammatory responses, tissue injury, and in various pathological conditions, including cancer. In tumor microenvironments, COX-2 overexpression leads to increased production of pro-inflammatory and pro-angiogenic prostaglandins, which foster tumor cell proliferation, survival, invasion, and metastasis. By selectively inhibiting COX-2, NSAIDs can disrupt these pro-oncogenic pathways. Most conventional NSAIDs, including ibuprofen, are non-selective, inhibiting both COX-1 and COX-2. This dual inhibition explains the recommendation to consume these medications with food to mitigate potential gastrointestinal side effects stemming from COX-1 suppression.
Emerging Evidence: Ibuprofen and Endometrial Cancer
Recent epidemiological investigations have brought into focus the specific potential of ibuprofen in modulating the risk of endometrial cancer. Endometrial cancer, originating in the lining of the uterus, represents the most prevalent gynecological malignancy in many developed nations, primarily affecting postmenopausal women. A comprehensive analysis, such as that derived from the Prostate, Lung, Colorectal, and Ovarian (PLCO) study, meticulously tracked health data from over 42,000 women aged 55 to 74 over a 12-year period. The findings revealed a statistically significant association: women who reported consistent monthly intake of at least 30 ibuprofen tablets exhibited a 25% lower probability of developing endometrial cancer compared to those consuming fewer than four tablets per month. This protective association was particularly pronounced within the subgroup of women concurrently diagnosed with heart disease, suggesting complex interactions between inflammatory pathways, cardiovascular health, and cancer susceptibility.
Endometrial cancer risk factors are well-documented and often involve hormonal imbalances and metabolic dysregulation. Obesity and overweight status are prominent risk factors, primarily due to excess adipose tissue leading to elevated estrogen levels. Estrogen can stimulate endometrial cell proliferation, thereby increasing the risk of malignant transformation. Other contributing factors include advanced age, certain types of hormone replacement therapy (particularly estrogen-only regimens), diabetes, and polycystic ovary syndrome. Early menarche, late menopause, and nulliparity also contribute to heightened risk. The potential role of ibuprofen in mitigating this risk may lie in its ability to counter the pro-inflammatory and proliferative signals often associated with these underlying conditions.
It is noteworthy that other common NSAIDs, such as aspirin, did not consistently demonstrate the same protective association with endometrial cancer risk in this particular study or in several related investigations. This observation underscores the potential for distinct pharmacological nuances and target specificities among different NSAID compounds, highlighting that a class effect cannot be universally assumed across all cancer types. Aspirin, while not showing a strong link to endometrial cancer prevention, has a well-established role in reducing the risk of colorectal cancer recurrence and is being investigated for other cancer types. Similarly, other NSAIDs like naproxen have been explored for their chemopreventive efficacy in various malignancies, including colon, bladder, and breast cancers, with outcomes often dependent on the specific cancer type, genetic predispositions, and individual health profiles.
Broader Chemopreventive Horizons
The potential benefits of ibuprofen appear to extend beyond endometrial cancer, encompassing a spectrum of other malignancies. Observational studies and preclinical investigations have linked its regular use to a reduced incidence or improved prognosis in bowel, breast, lung, and prostate cancers. For instance, individuals with a history of bowel cancer who incorporated ibuprofen into their regimen demonstrated a decreased likelihood of disease recurrence. Furthermore, laboratory studies have shown ibuprofen’s capacity to inhibit the proliferation and enhance the apoptosis of colon cancer cells. Intriguing preliminary data even suggest a protective effect against lung cancer in populations with increased risk, such as smokers.

Beyond its direct inhibition of COX enzymes, ibuprofen exerts pleiotropic effects that contribute to its anti-cancer potential. By reducing the production of prostaglandins, which are potent mediators of inflammation and cellular proliferation, ibuprofen directly impedes the growth and survival pathways of cancer cells. Lowered prostaglandin levels can thus hinder tumor initiation and progression.
Moreover, ibuprofen appears to modulate the activity of critical cancer-related genes and signaling pathways. These include Hypoxia-Inducible Factor 1-alpha (HIF-1α), Nuclear Factor-kappa B (NFκB), and Signal Transducer and Activator of Transcription 3 (STAT3). These transcription factors are frequently overexpressed or hyperactive in various cancers, playing pivotal roles in tumor angiogenesis, metabolism, immune evasion, and resistance to therapy. By downregulating their activity, ibuprofen may render cancer cells more susceptible to therapeutic interventions and less capable of thriving in challenging microenvironments. Additionally, research indicates that ibuprofen can influence epigenetic mechanisms, specifically altering the packaging of DNA within cells. This epigenetic modulation could potentially sensitize cancer cells to the effects of chemotherapy, improving treatment efficacy.
A Measured Perspective: Risks, Conflicting Data, and Clinical Imperatives
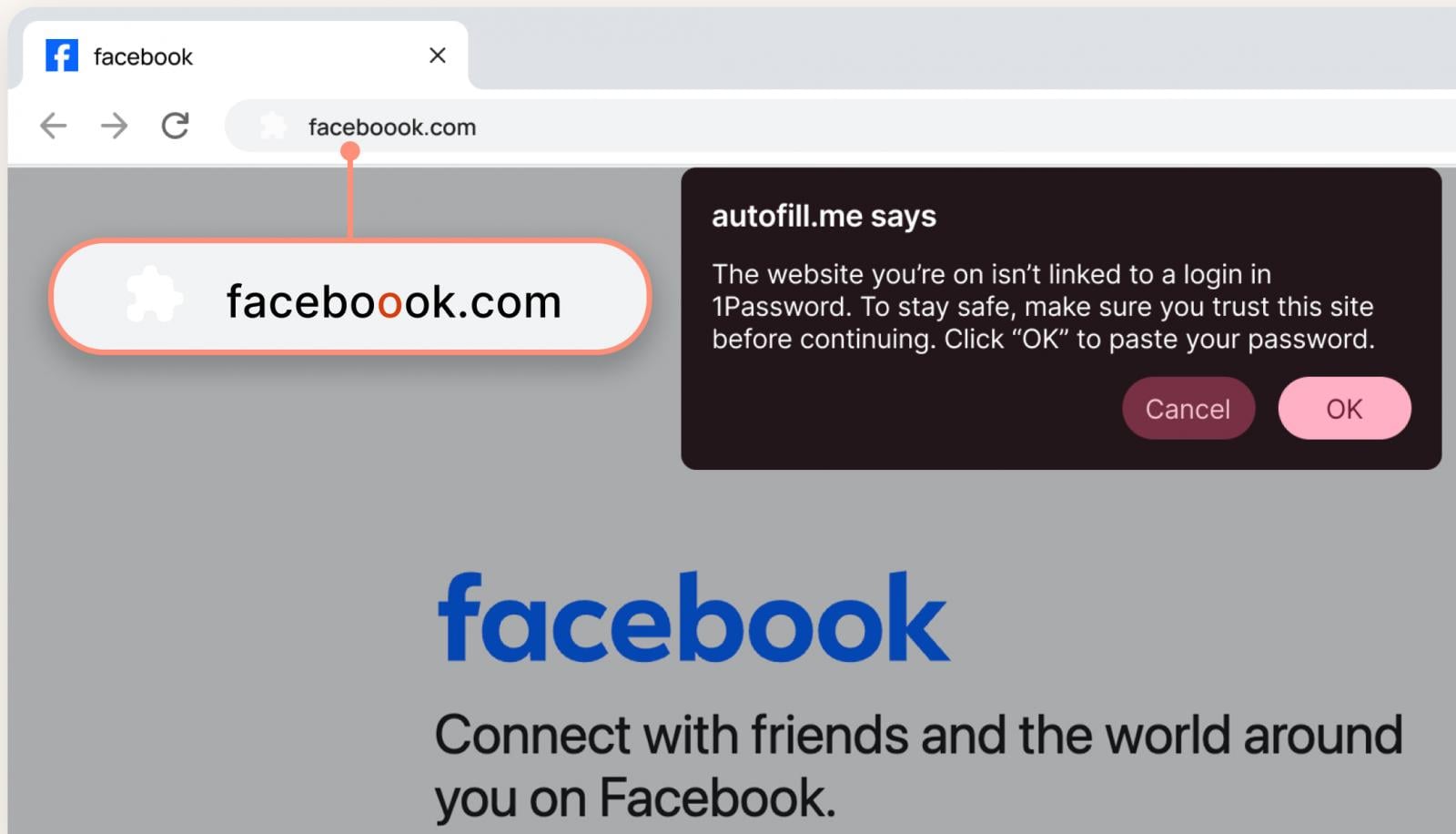
Despite the compelling biological rationale and emerging epidemiological evidence, the proposition of utilizing ibuprofen for cancer prevention necessitates a cautious and critically analytical approach. The scientific landscape surrounding NSAIDs and cancer risk is complex, characterized by some conflicting findings that underscore the need for further elucidation. For example, one study involving a substantial cohort of endometrial cancer patients suggested that aspirin use post-diagnosis, particularly among those with prior aspirin exposure, was associated with higher mortality rates. Other NSAIDs in that study also appeared to elevate cancer-related death risk.
Conversely, a more recent systematic review acknowledged the potential of NSAIDs, especially aspirin, in reducing the risk of several cancers, while simultaneously noting that regular use of other NSAIDs might be linked to an increased risk of kidney cancer. These disparate findings highlight the intricate and context-dependent interactions among inflammation, immunity, specific drug compounds, and the heterogeneous nature of cancer itself. The precise mechanisms governing these varied outcomes, including differences in dose, duration, patient demographics, and genetic predispositions, remain areas of active investigation.
The long-term or high-dose use of NSAIDs, including ibuprofen, is associated with a spectrum of well-documented and potentially serious adverse effects. These include significant gastrointestinal complications such as dyspepsia, gastritis, peptic ulcers, and potentially life-threatening gastrointestinal bleeding or perforation. Renal complications, including acute kidney injury and chronic kidney disease, can also occur, particularly in individuals with pre-existing renal impairment or those on concomitant medications that affect kidney function. Cardiovascular risks, such as an increased incidence of thrombotic events (e.g., heart attacks and strokes) and elevated blood pressure, are also recognized concerns, especially with prolonged use or in vulnerable populations.
Furthermore, NSAIDs are known to interact with numerous other medications. Concurrent administration with anticoagulants like warfarin can significantly amplify the risk of bleeding. Interactions with certain antihypertensive drugs, diuretics, and selective serotonin reuptake inhibitors (SSRIs) can lead to reduced drug efficacy or increased toxicity. These complex pharmacological interactions necessitate careful medical oversight, particularly in older patients or those with multiple comorbidities.
Future Directions and Responsible Application
The prospect of repurposing a common and affordable medication like ibuprofen for cancer prevention is undeniably exciting and holds immense potential for global public health. However, the current body of evidence, while suggestive, is predominantly derived from observational studies, which can identify associations but cannot definitively establish causation. To transition these findings into clinical recommendations, rigorous prospective randomized controlled trials are indispensable. Such trials would meticulously evaluate efficacy, optimal dosing regimens, treatment duration, and critically, the long-term safety profile of ibuprofen in specific high-risk populations.
Future research efforts should also focus on identifying biomarkers that can predict which individuals are most likely to benefit from ibuprofen’s chemopreventive effects, while simultaneously minimizing adverse reactions. Personalized medicine approaches, incorporating genetic and molecular profiling, could help tailor preventative strategies. The development of novel NSAID derivatives with enhanced anti-cancer specificity and improved safety profiles also represents a promising avenue.
Until such definitive evidence emerges, medical consensus firmly advocates for adherence to established, lifestyle-based cancer prevention strategies. These include maintaining a healthy body weight, engaging in regular physical activity, adopting a balanced diet rich in anti-inflammatory foods, and avoiding tobacco and excessive alcohol consumption. These foundational preventative measures remain the most robust and evidence-based approaches to reducing overall cancer risk.
In conclusion, the burgeoning scientific inquiry into ibuprofen’s potential role in cancer risk modulation represents a significant and promising area of research. While the idea that a ubiquitous painkiller could possess profound chemopreventive properties is captivating, the journey from observational association to clinical recommendation is long and fraught with complexities. For the present, individuals should refrain from self-medicating with ibuprofen for cancer prevention. All decisions regarding long-term medication use, particularly for preventative purposes, must be made in close consultation with a qualified healthcare professional, who can meticulously weigh the potential benefits against the inherent risks for each individual patient. The scientific community continues its diligent work to unravel these complexities, aiming to harness the full potential of existing compounds for future health benefits.